Osteoporosis means "porous bone." It is a condition that develops when more bone calcium is absorbed than is replaced in the normal bone remodeling process. Several factors contribute to the development of osteoporosis, but the exact reason why the remodeling process becomes unbalanced is unknown. Factors that often lead to osteoporosis include aging, physical inactivity, reduced levels of estrogen, excessive cortisone or thyroid hormone, smoking, and excessive alcohol intake. Loss of bone calcium accelerates in women after menopause.
Bone loss occurs most frequently in the spine, lower forearm above the wrist, and upper femur or thigh, the site where hip fractures usually occur.
Standard Definitions for Osteoporosis Diagnosis:
Low bone mass: A value for bone mineral density more than 1 standard deviation (SD) below the young female adult mean but less than 2.5 SD below this value.1
Osteoporosis: A value for bone mineral density 2.5 SD or more below the young female adult mean.2
Young female adult mean and standard deviation (SD): For the femoral neck, the mean and SD were based on data for 20- to 29-year-old non-Hispanic white females from the Third National Health and Nutrition Examination Survey (NHANES III).3 For the lumbar spine, the mean and SD were based on data for 30-year-old white women from the dual-energy x-ray absorptiometry (DEXA) densitometer manufacturer.4
Other races: People from racial and ethnic groups other than non-Hispanic white, non-Hispanic black, or Mexican American. This group consists primarily of Hispanic descent other than Mexican American, Asian, Native American, and multiracial persons, among others.
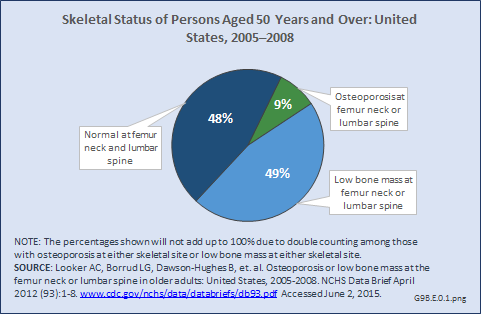
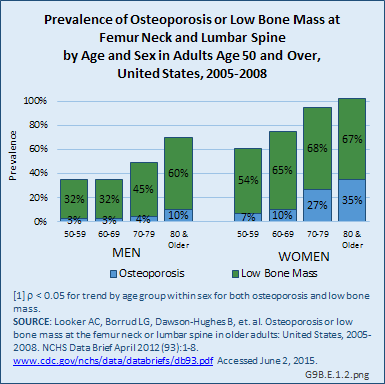
Nine percent of people aged 50 years and older had osteoporosis at either the femur neck or lumbar spine from 2005 to 2008 (Figure 1). Roughly one-half of older adults in the population had low bone mass at either the femoral neck or lumbar spine. Forty-eight percent of older adults in the United States had normal bone density at both the femur neck and lumbar spine.
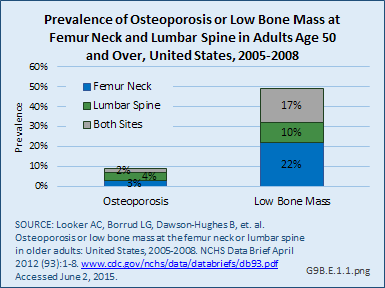
From 2005 to 2008, the prevalence of osteoporosis in women aged 50 years and older at either the femur neck or lumbar spine was 9%, with 4% with osteoporosis at the lumbar spine only, 3% with osteoporosis at the femur neck only, and 2% with osteoporosis at both the lumbar spine and femur neck. The prevalence of low bone mass at either skeletal site was 49%, with 10% having low bone mass at the lumbar spine, 22% with low bone mass at the femur neck, and 17% with low bone mass at both the lumbar spine and femur neck.
Age is a significant factor in the presence of osteoporosis and low bone mass in both men and women, but particularly in women. By the age of 70 years, virtually all women have low bone mass, with 27% or more having osteoporosis. In men, the prevalence of osteoporosis does not begin to increase until the age of 80 years, although low bone mass begins to climb for men in their 70s.
Osteoporosis often is not the principal diagnosis code related to a healthcare visit because the condition is usually an underlying cause of another condition, in particular, fragility fractures that often occur after a fall or other seemingly minor incident. Many times in such healthcare visits, osteoporosis may not even be listed as a condition. Still, in 2011, primary osteoporosis was listed in 1.8 million hospital discharges and emergency department visits as a reason for the visit in the population aged 50 and over. Fragility fractures occurred in 1.2 million visits for people aged 50 years and older. (Reference Table 9B.5 PDF [2] CSV [3])
Age is a factor in both primary osteoporosis diagnosis and in the occurrence of fragility fractures with most occurring in people after the age of 70. Nearly three-fourths (72%) of primary osteoporosis diagnoses were for people ages 70 years and older. However, in 2011, 9% of osteoporosis diagnoses was for people aged 50 to 59 years, and 19% of those aged 60 to 69 years. Among fragility fractures, 66% were for people aged 70 years and older, with the remainder split among those aged 50 to 69. The site of the fracture was particularly important with respect to age. The oldest group, those 70 years and older, were prone to fractures of the hip and vertebrae, as well as stress and pathological fractures. Fractures of the wrist and ankle or foot occurred across all people over the age of 50.
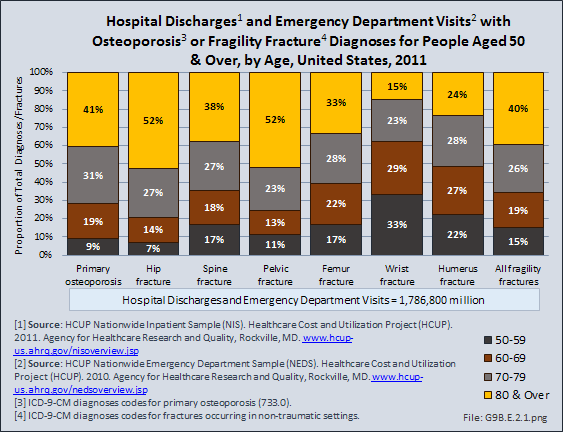
For 340,400 emergency department visits or hospital discharges for fragility fractures, or 16%, primary osteoporosis was also listed as a condition. The rate at which both diagnoses were made rose steadily as the population aged. Hospital discharge visits were more likely to include both primary osteoporosis and a fragility diagnosis than were visits to an emergency department.
Fractures are associated with significant increases in health services utilization compared to prefracture levels. Relative to the prior 6-month period, rates of acute hospitalization are between 19.5 (distal radius/ulna) and 72.4 (hip) percentage points higher in the 6 months after fractures. Average acute inpatient days are 1.9 (distal radius/ulna) to 8.7 (hip) higher in the postfracture period. Fractures are associated with large increases in all forms of postacute care, including postacute hospitalizations (13.1% to 71.5%), postacute inpatient days (6.1% to 31.4%), home health care hours (3.4% to 8.4%), and hours of physical (5.2% to 23.6%) and occupational (4.3% to 14.0%) therapy. Among patients who were initially community dwelling at the time of the initial fracture, 0.9% to 1.1% were living in a nursing home 6 months after the fracture. These rates rose by 2.4% to 4.0% one year after the fracture.1
INSTITUTIONALIZATION
Since 1980, there has been a nearly 15% decrease in the prevalence of chronic disability and institutionalization among people aged 65 years and older. A drop in disability translates directly into cost savings since it is seven times more expensive to care for a disabled senior versus a healthy one. Major activity limitations are a common cause of nursing home admissions. While the most common cause of limitations is arthritis, affecting nearly 50% of people older than 65 years and an estimated 60 million by 2020.2 Hip fractures are a second source of immobility, and are projected to reach 289,000 in the year 2030, nearly all fall-related.3
FRACTURES AND MORTALITY
Vertebral and hip osteoporotic fractures result in a 20% increase in mortality, usually observed in the 12 months after the fracture. Men, who are generally older at the time of the hip fracture, have a 30% mortality rate after the fracture. Moreover, comorbidities such as cardiovascular disease contribute to a higher mortality rate.
A population-based study in Olmsted County, MN, found that within the first seven days after hip fracture repair, 116 (10.4%) of participants experienced myocardial infarction and 41 (3.7%) subclinical myocardial ischemia. Overall, the 1-year mortality was 22%, with no difference between those with subclinical myocardial ischemia and those with no myocardial ischemia. One-year mortality for those with a myocardial infraction was significantly higher (35.8%) than for the other two groups.4 The relative mortality after vertebral fracture varies from 1.2 to 1.9 in different reports,5,6 but the excess deaths occur late, rather than early, after vertebral fractures.5
Links:
[1] http://www.nia.nih.gov/newsroom/features/nih-seeking-strategies-multiple-chronic-conditions-older-people
[2] https://bmus.latticegroup.com/docs/T9B.5.pdf
[3] https://bmus.latticegroup.com/docs/T9B.5.csv
[4] http://www.agingsociety.org/agingsociety/publications/chronic/index.html
[5] http://www.cdc.gov/HomeandRecreationalSafety/Falls/adulthipfx.html